One-Size-Fits-All Immunotherapy for Pancreatic Cancer Developed Dr. Yang & Team

Pancreatic cancer is among the deadliest forms of cancer, with most patients diagnosed after the disease has already spread throughout the body. The five-year survival rate for metastatic cases hovers around 2–3%, and median survival is often measured in months rather than years.
Now, Dr. Lili Yang and UCLA researchers have engineered a novel immunotherapy that could offer new hope for a disease that has remained stubbornly resistant to treatment advances for decades. In a study published in PNAS, the team details how the therapy, called CAR-NKT cell therapy, can track down and destroy pancreatic tumors even after they’ve metastasized to other organs.
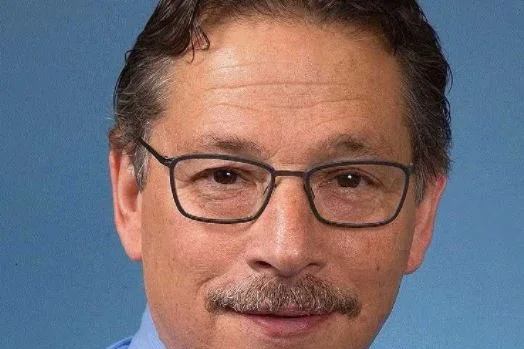
“Developing a therapy that targets both the primary tumor and its metastases in preclinical studies — one that can be ready to use off-the-shelf — represents a fundamental shift in how we might treat this disease,” said senior author Dr. Lili Yang, a professor of microbiology, immunology and molecular genetics and a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA.
The therapy uses engineered immune cells that can be mass-produced from donated blood stem cells and stored ready-to-use. This approach offers an immediately available treatment option at approximately $5,000 per dose — a fraction of the cost of current personalized cell therapies, which can run hundreds of thousands of dollars and require weeks of manufacturing time that many pancreatic cancer patients simply don’t have.